Can I conserve breast?
Is it safe?
After confirming cancer, doing the staging and fitness and making a decision, we have finally reached the point, where treatment starts. For the sake of discussion, we are assuming, it's a small cancer in early stage, and the first step is surgery. The decision about type of surgery is a very delicate one. But then, it is rather straight forward. The principle is clear - we encourage to conserve the breast wherever possible. Only where conservation is not possible, we go ahead with removal. Of course, the patient's choice is supreme, and there are times, when conservation is possible, but patients opt for removal. That's an indivdual call.
A surgery for breast cancer, has two parts to be tackled:
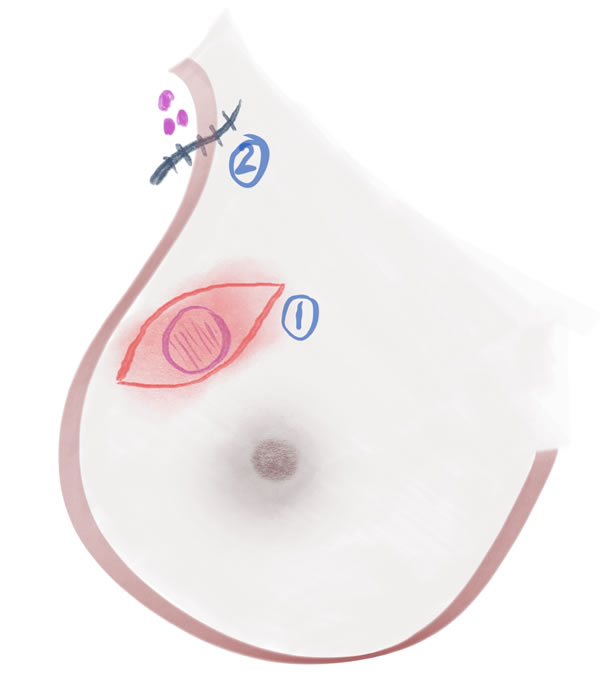
1. The Tumour in Breast
2. The Nodes in the Armpit (Axilla)
For point 1. above, for operating the tumour in the breast, there are two options:
1. We remove the whole breast - This is called as Mastectomy
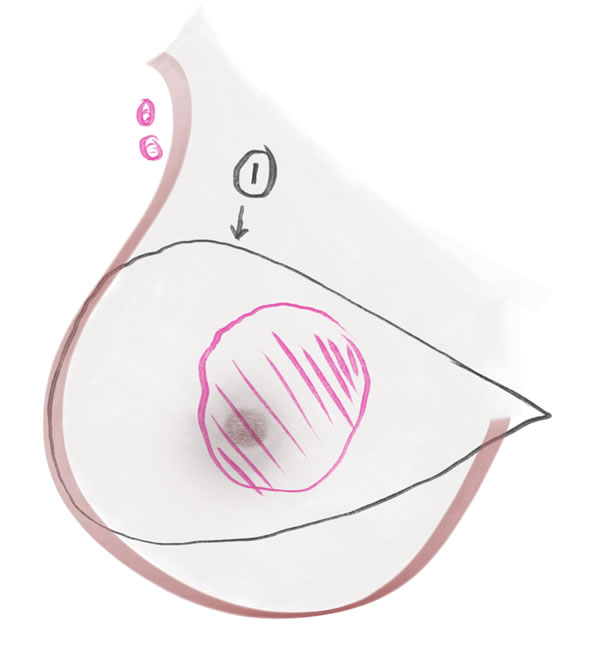
2. We do not remove the whole breast. We remove only the tumour, with a cuff of one centimetre of normal tissue around it - This is called as Breast Conserving Surgery
In both the surgeries above, the nodes in the armpit have to be removed, as per the stage. In cases where the nodes are definitely 'involved', we remove all of them. When the nodes are not looking involved, we remove only a few of them and test (by a technique called Sentinel Node Biopsy and Frozen Section) - if they turn out 'negative' for cancer, we just leave behind the rest; and if they test 'positive' for cancer, then we remove them all.
Is it safe doing a Breast Conserving Surgery (BCS)? Isn't there a higher chance of the cancer coming back?
A Breast Conserving Surgery (BCS) is absolutely safe. The one point that most patients think is that, not removing the breast will cause a higher chance of the cancer coming back. But this is not correct. To explain, let's first discuss - how and where does a cancer come back?
A breast cancer can 'come back' (recur) in two ways:
1. 'Locally' - around the same area, where the breast is or the breast was.
2. 'Distant' - elsewhere - liver, lung, bone, nodes around the windpipe, in the abdomen, brain, anywhere basically.
A 'Local Recurrence' still has a chance of cure. A 'Distant Recurrence' would be near impossible to cure.
So understanding the 'recurrence' above, please note this statement: If the surgery is done by a Qualified Surgical Oncologist, whether the breast is removed (Mastectomy) or the breast is not removed (Breast Conserving Surgery), the chances of a 'Distant Recurrence' are the same (there is no difference); but, the chances of 'Local Recurrence' are more if the breast is not removed as compared to when it is removed. One should not worry much about this 'local recurrence' part and definitely opt for a Breast Conserving Surgery (if surgically feasible); in BCS, we compulsorily give Radiation to the breast which will reduce chances of cancer coming back 'locally' and besides, the patient is on a regular follow up with us, so that, in case, something comes up in the breast, we can always treat again.
So now that we have sorted out the issue of recurrence, let's focus on surgeries for breast cancer:
1. Breast Conservative Surgery - Breast is not removed
2. Modified Radical Mastectomy - Breast is removed
3. Reconstruction - Some additional surgery is done to re create the breast.